Tempramed Blog
Why Your Blood Sugar Spikes Might Be Caused by Damaged Insulin
Sarah checked her blood glucose meter three times, certain it was malfunctioning. Despite taking her usual insulin dose, her reading showed 287 mg/dL, nearly double her target range. She'd been managing Type 1 diabetes for 15 years and knew her body well. Something was definitely wrong.
After ruling out illness, stress, and carbohydrate miscounting, Sarah discovered the culprit: her insulin pen had been sitting in her car's glove compartment during a scorching summer afternoon. The damaged insulin had lost its effectiveness, causing dangerous blood sugar spikes despite proper dosing.
If you're experiencing unexplained high blood glucose readings despite consistent diabetes management, damaged insulin might be the hidden culprit. This often-overlooked cause affects thousands of people with diabetes annually, leading to frustrating insulin not working scenarios that can feel impossible to solve.
The Hidden Reality of Insulin Degradation
Damaged insulin symptoms are often mistaken for other diabetes management issues, leading to unnecessary medication adjustments, increased stress, and potentially dangerous complications. Unlike obvious medication problems like expired prescriptions or empty pens, insulin degradation can be invisible to the naked eye while completely destroying medication effectiveness.
Recent studies show that up to 30% of insulin effectiveness can be lost within just two hours of exposure to temperatures above 86°F (30°C). Even more concerning, insulin exposed to freezing temperatures becomes permanently inactive, even after returning to room temperature. These scenarios create the perfect storm for blood sugar spikes that resist standard treatment approaches.
The financial impact compounds the health risks. With insulin costs averaging $50-$300 per pen, damaged medication represents significant monetary loss. More critically, using ineffective insulin can lead to diabetic ketoacidosis (DKA) in people with Type 1 diabetes, a potentially life-threatening emergency.
Understanding Insulin Degradation: The Science Behind the Problem
Insulin is a complex protein hormone consisting of 51 amino acids arranged in a precise three-dimensional structure. This delicate molecular architecture makes insulin remarkably effective for blood sugar control but equally vulnerable to environmental damage.
How Temperature Damages Insulin
Heat exposure above 86°F (30°C):
-
Protein molecules begin unfolding (denaturation)
-
Chemical bonds maintaining insulin structure break down
-
Irreversible aggregation creates inactive clumps
-
Degradation accelerates exponentially with higher temperatures
Cold damage below 36°F (2°C):
-
Ice crystal formation physically destroys protein structure
-
Freezing damage occurs even with brief exposure
-
Thawed insulin appears normal but is completely inactive
-
No visual indicators reveal the damage
Environmental Factors Accelerating Degradation
Light exposure:
-
Ultraviolet radiation breaks peptide bonds
-
Fluorescent lighting contributes to gradual potency loss
-
Direct sunlight causes rapid deterioration
-
Even indirect light exposure reduces effectiveness over time
Physical agitation:
-
Vigorous shaking denatures protein molecules
-
Constant vibration during transport affects stability
-
Air bubbles from shaking interfere with accurate dosing
-
Proper mixing requires gentle rolling, never shaking
Recognizing Damaged Insulin: Warning Signs and Symptoms
Physical Appearance Changes
It is important to note that in most cases, there will be no physical signs of damaged insulin, and the medication will not indicate visible changes. But if you see any of the following, it is important to replace the insulin:
-
Any cloudiness or discoloration indicates damage
-
Floating particles or visible clumps
-
Crystalline formations on container walls
-
Color changes from crystal clear appearance
Cloudy insulins (NPH and premixed):
-
Clumping that persists despite gentle mixing
-
Unusual separation patterns
-
Crystalline deposits that won't dissolve
-
Dramatic color changes from normal appearance
Performance-Based Warning Signs
Unexpected blood glucose patterns:
-
Blood sugar spikes despite proper dosing and timing
-
Gradual increase in insulin requirements without explanation
-
Unpredictable glucose responses to familiar meals
-
Resistance to correction doses that previously worked effectively
Physical symptoms indicating insulin not working:
-
Increased thirst and frequent urination
-
Persistent fatigue despite adequate sleep
-
Blurred vision developing over hours or days
-
Ketones in urine (particularly dangerous for Type 1 diabetes)
Critical Emergency Indicators
Seek immediate medical attention if experiencing:
-
Blood glucose readings above 300 mg/dL (16.7 mmol/L)
-
Vomiting or inability to keep fluids down
-
Signs of diabetic ketoacidosis (fruity breath, rapid breathing)
-
Severe dehydration or altered mental status
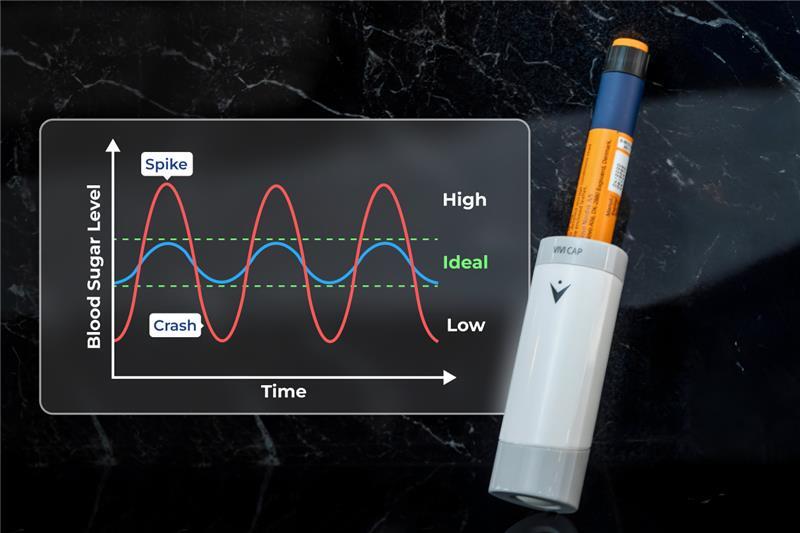
The Cascade Effect: How Damaged Insulin Compounds Problems
When insulin loses effectiveness, people with diabetes often respond by increasing doses, creating a dangerous cycle of problem-solving attempts that can worsen the situation.
Common Counterproductive Responses
Dose escalation:
-
Taking larger amounts of ineffective insulin provides no benefit
-
Increased injection frequency using damaged insulin remains ineffective
-
Stack-dosing with compromised medication can lead to delayed hypoglycemia when effective insulin is finally used
-
Growing frustration and anxiety about diabetes management
Dietary restrictions:
-
Unnecessary food limitations when insulin is the actual problem
-
Increased stress about carbohydrate intake
-
Social isolation from meal-related activities
-
Nutritional imbalances from overly restrictive eating
Healthcare System Interactions
Misdiagnosis scenarios:
-
Healthcare providers may suspect medication non-compliance
-
Insulin resistance diagnosis when storage is the actual issue
-
Unnecessary medication changes or additions
-
Increased healthcare costs from treating symptoms rather than causes
Advanced Storage Solutions: Preventing Insulin Damage
Modern technology has revolutionized insulin storage, eliminating traditional refrigeration dependence while providing superior protection against temperature extremes.
Phase Change Material (PCM) Technology
Professional storage solutions now utilize space-grade materials that maintain optimal insulin temperatures without external power sources. These systems automatically absorb or release heat during material phase transitions, creating self-regulating temperature environments.
Technology advantages:
-
No electrical power requirements or battery maintenance
-
Compact designs that fit in pockets or small bags
-
Extended protection lasting 24-48 hours in extreme conditions
-
Effective temperature range from -4°F to 140°F (-20°C to 60°C)
The VIVI Cap Solution
The VIVI Cap represents the gold standard in insulin temperature protection, utilizing patented PCM technology originally developed for space applications. This innovative solution addresses every major cause of insulin degradation:
Temperature protection:
-
Maintains optimal insulin storage temperature in extreme heat or cold
-
Self-regulating system prevents overheating and freezing
-
No maintenance required, works automatically 24/7/365
-
Tested and validated in temperatures from -4°F to 140°F
Light protection:
-
Opaque design shields insulin from harmful UV radiation
-
Protects against fluorescent and LED lighting damage
-
Maintains insulin potency during extended storage periods
-
Professional-grade protection equivalent to original packaging
Physical protection:
-
Cushioned interior prevents agitation damage
-
Secure closure prevents accidental opening
-
Compact design fits easily in pockets, purses, or bags
-
TSA-approved for air travel without restrictions
Real-World VIVI Cap Performance
Independent testing validates VIVI Cap effectiveness across extreme conditions that would destroy unprotected insulin within hours. Users report consistent blood sugar control regardless of environmental challenges, from desert heat exceeding 120°F to winter temperatures below freezing.
The customer testimonials consistently highlight the peace of mind that comes from reliable insulin protection, allowing people with diabetes to focus on living their lives rather than constantly worrying about medication storage.
Taking Action: Your Step-by-Step Solution Plan
Immediate Assessment (Next 24 Hours)
Evaluate current insulin storage:
-
Check where you store unopened and in-use insulin
-
Identify potential temperature exposure sources
-
Review recent blood glucose patterns for unexplained spikes
-
Examine insulin appearance for visual degradation signs
Test storage locations:
-
Use a thermometer to measure actual temperatures in storage areas
-
Monitor temperature variations throughout the day
-
Check car, office, and travel storage conditions
-
Document findings to identify problem areas
Short-Term Solutions (This Week)
Improve current storage:
-
Move insulin away from heat sources, windows, and bright lights
-
Verify refrigerator temperatures are between 36-46°F (2-8°C)
-
Create dedicated, protected storage areas for in-use insulin
-
Establish backup storage protocols for different scenarios
Replace questionable insulin:
-
Discard any insulin showing visual signs of degradation
-
Replace insulin that may have been exposed to temperature extremes
-
Start fresh with properly stored supplies
-
Monitor blood glucose closely with new insulin supplies
Long-Term Prevention Strategy
Invest in professional storage:
-
Consider temperature-controlled storage solutions like the VIVI Cap
-
Evaluate storage needs for home, work, travel, and emergency situations
-
Calculate cost-benefit of prevention versus replacement and health risks
-
Plan for various scenarios: power outages, travel, seasonal changes
Develop monitoring systems:
-
Create routine checks for insulin storage conditions
-
Establish blood glucose monitoring protocols to detect early degradation
-
Document patterns that might indicate storage problems
-
Build relationships with healthcare providers for guidance and support
Emergency Preparedness
Create backup systems:
-
Maintain extra insulin supplies stored in optimal conditions
-
Develop emergency protocols for storage system failures
-
Establish relationships with local pharmacies for urgent replacements
-
Prepare emergency contacts and medical documentation for travel
Education and awareness:
-
Share knowledge with family members and caregivers
-
Educate workplace colleagues about proper insulin storage
-
Understand insurance coverage for storage-related medication replacement
-
Stay informed about new storage technologies and best practices
The Economics of Prevention
Investing in proper insulin storage provides substantial financial returns beyond health benefits. Professional storage solutions typically cost $150-$300 but prevent thousands of dollars in medication replacement, healthcare costs, and productivity losses.
Cost analysis:
-
Average insulin replacement due to storage damage: $500-$2,000 annually
-
Emergency healthcare costs from damaged insulin complications: $1,000-$5,000+
-
Professional storage system investment: $150-$300 (one-time)
-
Return on investment timeline: 3-6 months
Beyond financial considerations, proper storage eliminates the stress, anxiety, and lifestyle limitations associated with constant worry about insulin effectiveness. The freedom to travel, work, and live normally without medication concerns is invaluable.
Conclusion: Take Control of Your Insulin's Effectiveness
Blood sugar spikes caused by damaged insulin represent a preventable but widespread problem affecting thousands of people with diabetes. Understanding the science behind insulin degradation, recognizing warning signs, and implementing proper storage solutions can eliminate this hidden threat to your health.
The solution is straightforward: protect your insulin with the same care you give other critical aspects of diabetes management. Professional storage systems like the VIVI Cap provide reliable, maintenance-free protection that eliminates storage-related insulin degradation.
Key takeaways:
-
Insulin degradation often causes unexplained blood sugar spikes
-
Temperature, light, and agitation can destroy insulin effectiveness
-
Visual inspection alone cannot detect all insulin damage
-
Professional storage solutions provide comprehensive protection
-
Prevention costs far less than replacement and complication treatment
Don't let damaged insulin sabotage your diabetes management. Take action today to protect your medication, your health, and your peace of mind. With proper storage, you can trust that your insulin will work when you need it most, providing the consistent blood sugar control essential for living your best life with diabetes.